As you're considering which employee perks to include in your benefits package, don't sleep on fertility assistance.
The World Health Organization (WHO) estimates that 17.5% of the global adult population experience infertility. Honing in on the United States, 19% of married women aged 15 to 49 with no prior births are unable to achieve pregnancy after one year of trying, according to the Centers for Disease Control and Prevention (CDC). Of course, single parents and same-sex couples also struggle with fertility and family planning.
While everyone on this journey faces different emotional and legal challenges, the financial burden is universal. More than 80% of people who undergo fertility treatments have little to no insurance coverage, according to the 2021 FertilityIQ Workplace Index.
Infertility can weigh on a person's mind, impacting their performance in the workplace and even motivating them to switch employers or careers. However, HR leaders can help alleviate some of the stress of family planning by offering fertility benefits.
In this post, we'll cover:
- What are Fertility Benefits?
- Types of Fertility Benefits
- Why You Should Offer Fertility Benefits
- How to Maximize Your Fertility Benefits Package
What are Fertility Benefits?
Fertility benefits are employer-sponsored treatments and services that support family planning, such as assisted reproductive technology, which includes all fertility treatments in which eggs or embryos are handled. Some examples are egg freezing, in vitro fertilization (IVF), and gestational surrogacy. Fertility benefits are sometimes referred to as family building benefits, although the latter is broader in scope.
The CDC defines these procedures as surgically removing eggs from a woman’s ovaries, combining them with sperm, and then either returning them to the woman’s body or donating them to another woman. Conversely, fertility treatments in which only sperm are handled, such as intrauterine insemination (IUI) or artificial insemination, are excluded.
Fertility services in general are on the rise, with 40% of U.S. companies currently offering fertility benefits, according to the International Foundation of Employee Benefit Plans (IFEBP). That's up 10% from 2020, indicating that the COVID-19 pandemic has prompted employers to increase their health benefits to focus on employees holistically. Furthermore, the U.S. Office of Personnel Management has announced that health insurance plans for federal employees will be expanded in 2024 to include coverage of more infertility treatments.
Although there's no federal law that requires employers to provide fertility benefits, there are currently 20 states that mandate some form of fertility coverage:
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Hawaii
- Illinois
- Louisiana
- Maine
- Maryland
- Massachusetts
- Montana
- New Hampshire
- New Jersey
- New York
- Ohio
- Rhode Island
- Texas
- Utah
- Virginia
Types of Fertility Benefits
The types of fertility benefits that employers offer vary widely depending on their health coverage. Below are examples of fertility services and treatments sometimes included in insurance plans:
Genetic testing

Many health insurance providers cover fertility testing, even if they don't cover fertility treatment. In fact, most health plans will include fertility services only if the patient has received an infertility diagnosis. Fertility testing can help employees learn not only when they're most likely to get pregnant, but also the causes of their infertility, such as genetics.
Doctors recommend genetic testing as part of pregnancy planning to determine if a patient or couple has recessive genes that could affect their offspring. Roughly 16% of U.S. employers currently cover genetic testing, which is up from 12% in 2020, according to the IFEBP.
Drug therapy
Depending on the infertility diagnosis, doctors may prescribe fertility drugs to help patients achieve pregnancy. Fertility medications can be quite costly, and some health plans may reduce employees' out-of-pocket medication costs. The IFEBP reports that 28% of U.S. employers currently cover fertility medications, more than triple the amount (8%) in 2016.
Fertility preservation
The National Institutes of Health (NIH) defines fertility preservation as the process of saving eggs, sperm, or reproductive tissue so that a person can use them to have biological children in the future. Fertility preservation procedures include egg freezing, sperm freezing, and embryo freezing. One of the fastest-growing family planning benefits, egg freezing is now offered by 14% of U.S. employers compared to just 2% in 2016, according to the IFEBP.
Third-party reproduction
Third-party reproduction is when eggs, sperm, or embryos have been donated by someone else to facilitate an infertile individual's pregnancy. Unfortunately, health plans rarely cover the cost of donor sperm or donor egg services, which can break the bank. While the cost of one vial of donor sperm generally ranges from $400 to $2,000, Forbes reported, the cost of a donor egg cycle can range from $15,000 to $20,000 and higher.
Intrauterine insemination (IUI)
Intrauterine insemination (IUI) is a form of artificial insemination, in which donor sperm or an intended parent's sperm is washed, concentrated, and implanted into the uterus around the time of ovulation. Before IUI, employees may take fertility medications to prepare their eggs. Less expensive than other fertility treatments, IUI generally costs between $300 and $1,000 without health insurance, according to Planned Parenthood.
In vitro fertilization (IVF)

Considered the most effective form of assisted reproductive technology by the Mayo Clinic, in vitro fertilization (IVF) is a multi-step process that involves retrieving eggs from ovaries and fertilizing them with sperm in a laboratory. Once the embryo is created, preimplantation genetic screening can be performed, ensuring that the embryo has the correct number of chromosomes. Finally, the embryo is ready to be transferred to the uterus.
One IVF cycle can last at least three weeks, if not longer when genetic testing is conducted. Also, employees may face clinic restrictions, such as age limits on allowing IVF treatment of women between the ages of 42 and 45 using their own eggs, according to the Advanced Fertility Center of Chicago.
Even though IVF success depends on a variety of factors, including age and overall health of the patient, cumulative pregnancy rates tend to increase after more than three cycles, according to UT Health San Antonio. That's quite the investment, though, as a single IVF cycle can cost anywhere from $15,000 to $30,000, with medication costs accounting for up to 35% of that sum, Forbes reported.
The number of U.S. employers offering IVF benefits has more than doubled since 2016, with 30% currently covering IVF treatment, according to the IFEBP.
Surrogacy services
Traditional surrogacy is when a woman is artificially inseminated with the father's sperm and then carries the baby to birth to give to the parents. Gestational surrogacy is when an embryo created from IVF is implanted in the uterus of a third-party, who carries the baby to birth to give to the parents.
Most employer-provided health insurance plans don't cover surrogacy services, so employees typically take out supplemental insurance policies. Insurance issues should be ironed out when negotiating the contract. As for total cost of surrogacy, including base compensation, insurance, and legal fees, experts estimate the process can cost anywhere between $100,000 and $200,000, according to U.S. News & World Report.
Adoption benefits

Family planning benefits may also focus on adoption. More than one third (34%) of U.S. employers currently offer paid parental leave and 22% offer unpaid parental leave for when employees adopt a child, according to the IFEBP. Meanwhile, nearly one in five (19%) offer financial assistance to cover adoption fees and legal expenses.
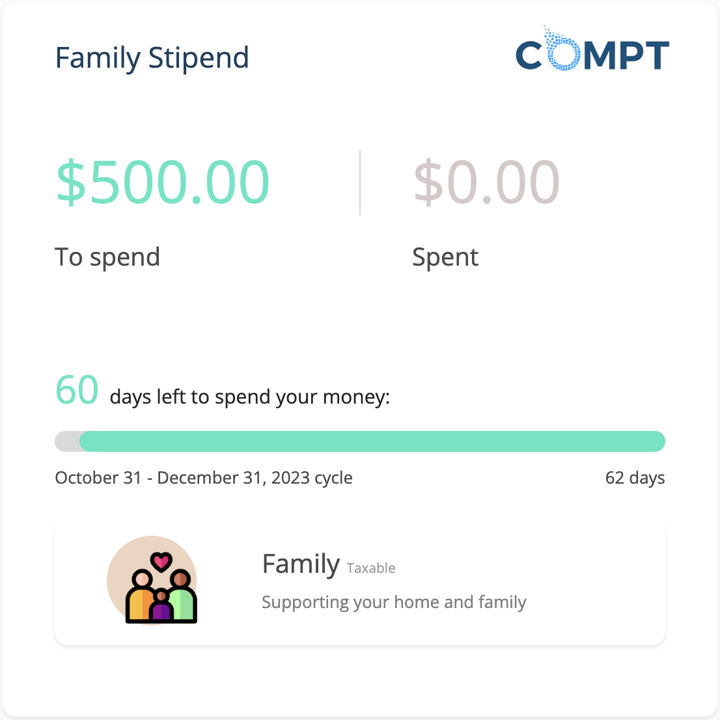
Family stipends
Compt, a 100% IRS-compliant reimbursement platform, helps companies offer inclusive, personalized, and flexible compensation and benefits programs, such as family stipends. They're sums of money given to employees in addition to regular wages to help them pay for family-related expenses, such as fertility treatments. Family stipends can also be used for surrogacy costs, adoption fees, and other fertility care expenses.
Why You Should Offer Fertility Benefits
Since the pandemic, HR leaders have been increasingly supporting employees in not only their careers, but also their personal lives. In order to provide comprehensive coverage for all of their physical, mental, and financial needs, companies need to offer fertility benefits.
Just 32% of employees around the world say they can afford fertility treatments if needed, according to the 2023 Global Fertility at Work report by Carrot Fertility. Meanwhile, 39% would have to dip into savings to afford fertility treatment and 29% may incur debt to pay for it.
That's because most insurance coverage doesn't include fertility care. And if it does, an infertility diagnosis is usually required, which excludes same-sex couples and people who want to be single parents. As a result, they have to spend a lot more money on fertility assistance – 63% of LGBTQ+ people planning families expect to use assisted reproductive technology, foster care, or adoption, according to a survey by Family Equality.
If your company is firmly committed to diversity, equity, and inclusion (DEI), you need to implement family-forming benefits without any strings attached. After all, these inclusive benefits promote economic equity in the workplace, with as many as 75% of employees considering fertility benefits to be an important part of an inclusive company culture, according to the Carrot report.
Family-planning benefits can also boost recruitment and retention. Taking into account the financial hurdles that people trying to start a family encounter, it's no surprise that 42% of job seekers say that a new job offer with no fertility benefits would be a “deal breaker," according to the Carrot report. Even 65% of current employees would switch jobs to work for an employer offering fertility benefits. Furthermore, nearly three quarters (72%) would stay at their company longer if they had access to fertility benefits.
In addition to lowering their attrition rate, organizations that offer fertility benefits experience higher employee engagement, morale, and productivity. Let's refer back to the Carrot report: More than half of employees (55%) say that fertility challenges have hindered their work performance, and 65% admit to spending time at work researching fertility treatments, fertility benefits, and family forming.
By alleviating some of the stress and anxiety associated with fertility care, HR leaders can bring relief to struggling employees, strengthening their concentration and resolve in the workplace. Best of all, 97% of employers who expanded their fertility coverage didn't experience a "significant increase" in health care costs, according to the National Infertility Association.
Real World Example of Fertility Benefits in Practice: Meaghan’s Story
Meet Compt's very own Senior Manager of Marketing Operations, Meaghan Ferneau—a shining example of how employee fertility benefits can truly make a difference in people's lives.
Previously, Meaghan faced hurdles with her former employer's insurance coverage when starting her family journey via IVF. Although she was offered "fertility coverage up to $10,000," most private fertility clinics didn't accept this coverage, leaving her responsible for the majority of the expenses incurred.
When she joined Compt in 2022, she was thrilled to learn that all employees have access to an annual $4,000 out-of-state care stipend—an attractive benefit for patients seeking assisted reproductive technology, as many travel across state lines for treatments. She subsequently used this benefit to defray the costs of clinic fees, travel, and room and board to her preferred IVF clinic in St. Louis, Missouri.
“Because of the flexibility of Compt’s out-of-state care stipend, I was reimbursed for a majority of expenses related to our third IVF transfer, which, up until that point, had been completely out-of-pocket. With Compt’s stipend, we could comfortably navigate through our third transfer round without worrying about how we would fare financially; making it an easy decision to move forward with another procedure.”
Thanks to this employee benefit, Meaghan's dream of starting her own family became a reality. In 2023, she and her husband welcomed their daughter, Zuzu. Her story serves as a testament to the transformative power of flexible fertility benefits.

How to Maximize Your Fertility Benefits Package
If you're truly invested in supporting employees with fertility issues, there are several ways you can administer fertility benefits.
Shop for all-encompassing health plans
Select a health insurance plan with comprehensive coverage of fertility services. That means avoiding any plan that requires an infertility diagnosis, which prevents same-sex couples and aspiring single parents from access to covered services most beneficial to their situations, like fertility preservation, artificial insemination, and IVF.
In order for these to be inclusive benefits, make sure the plan doesn't impose less invasive treatments before employees are eligible for IVF or IUI. You don't want employees to max out their coverage before it's time for the necessary procedure.
Expand your health insurance coverage
You can also partner with a third-party provider to supplement your existing health insurance plan with fertility coverage. Although a third-party provider comes with another price tag, the return-on-investment (ROI) will be worth it because your workforce will appreciate and value the wider range of covered services.
Give emotional support
Employees grappling with infertility challenges need all the help they can get. It's up to HR to provide emotional support, either through counseling and other mental health resources or an employee resource group (ERG). Consisting of team members who volunteer their time and effort to champion an inclusive workplace, ERGs are comprised of employees of a similar background or shared experience, such as infertility. ERGs promote camaraderie among different segments of the workforce, resulting in higher talent retention.
Be flexible
Family forming takes time, which is why employers should arrange flexible work schedules to accommodate employees' fertility health needs, like attending a doctor's appointment or taking foster kids to school. Other forms of flexibility can include remote work, parental leave, and even paid time off (PTO) for fertility treatments.
Final Thoughts
As the data indicates, fertility benefits are trending upward in this post-pandemic world. Innovative companies dedicated to DEI are making fertility services accessible to all employees, regardless of marital status, gender identity, and sexual orientation. If you want to compete for top talent in this highly competitive landscape, you need to evaluate your health insurance plan ASAP and optimize your family-building coverage.
With Compt, you can offer a fertility benefit stipend to your employees. To learn more, schedule a customized demo with us today.
